
Gum Inflammation and Disease Explained
Find out what inflammation is, how it works and how it relates to gum disease and your overall health

Gum inflammation? Like most people, you’ve probably come across the term “inflammation” before in relation to your whole body… but how does it occur? Are inflammation and infection related? Can it spread to the rest of your body? Inflammation is a pretty complex notion… which we’ve decided to demystify in this blog article! Read on to better understand what inflammation is and what it means for your gums, teeth and overall health.
Acute inflammation – a blessing in disguise!
Remember the last time you burnt your tongue, pulled a muscle or had a sore throat? Well, believe it or not, these all have one thing in common and that’s inflammation. Let us explain: when any of the body’s living tissues are damaged – through injury, germs, disease or a medical condition – an inflammatory-immune response is triggered to address the cause of damage and start the healing process [1].
Basically, what happens is that when the body perceives it is under attack, it mobilizes its resources – the immune cells that live in body tissue – to fight. A whole army of immune cells is recruited. To get reinforcement, immune cells release substances known as inflammatory mediators that attract other immune cells to the area. These reinforcement cells travel through the bloodstream and cross the vessels to get into the damaged tissue. To facilitate this process, blood vessels become bigger and more permeable, that’s why the affected area becomes red, hot and swollen [2]!This is known as acute inflammation.
Acute inflammation has two phases: the first involves fighting the cause of the damage and “cleaning up” the area, while the second is all about reconstructing the damaged tissue. It’s important to note that the body cannot move into phase two if phase one is still ongoing.
Even though it can be painful and sometimes look alarming, acute inflammation is in fact a vital mechanism for your health and well-being [3]. It is a vehicle to healing. Inflammation usually declares itself soon after the damage has occurred – within minutes or hours – and should be short-lived, subsiding once the affected area is “returned to a state of balance” [4]. It’s only if inflammation lingers and becomes chronic that it can become a burden for the body and your health.
What does this have to do with gum disease?
Gum disease = gum inflammation
When we talk about “gum disease”, what we’re actually on about is inflammation of the gums. Gingivitis, which is early-stage gum disease, literally means “inflammation of the gingiva”. As previously explained, inflammation occurs when living tissues have been damaged. In the context of gum disease, damage is often caused by plaque and tartar build-up [5] on the tooth surface, along the gum line which, because of poor oral hygiene, can lead to gingivitis. Indeed, when the bacteria in plaque release toxins which come into contact with the gums, this triggers an inflammatory-immune response.
As we said previously, acute inflammation is the body’s response to harmful stimuli – a defense mechanism – and is therefore welcome. Your immune system cells will tend to the affected area to repair the damage. However, it is important to address the root cause – in most cases, plaque build-up [6] – of the inflammation for gum health. In other words, to prevent it from lingering and getting worse.
From gingivitis to periodontitis – when inflammation turns nasty
While gingivitis is a reversible condition affecting up to 90% of the world’s adult population, it can progress. If left untreated, what started with the minor signs of gum disease - swollen gums, bleeding gums, bad breath - can lead to a more severe form of gum disease known as periodontitis. This condition is characterized by chronic inflammation. Unlike acute inflammation, which is short-lived and enables the healing process, chronic inflammation is persistent, inhibits healing and actually causes further damage [7]. Basically, with chronic inflammation, the first phase of “fighting and cleaning up” persists because the body is not able to address the initial cause of damage. In the case of periodontitis, the plaque and bacteria. As long as this phase is active, the body cannot move on to the second phase and reconstruct tissue.
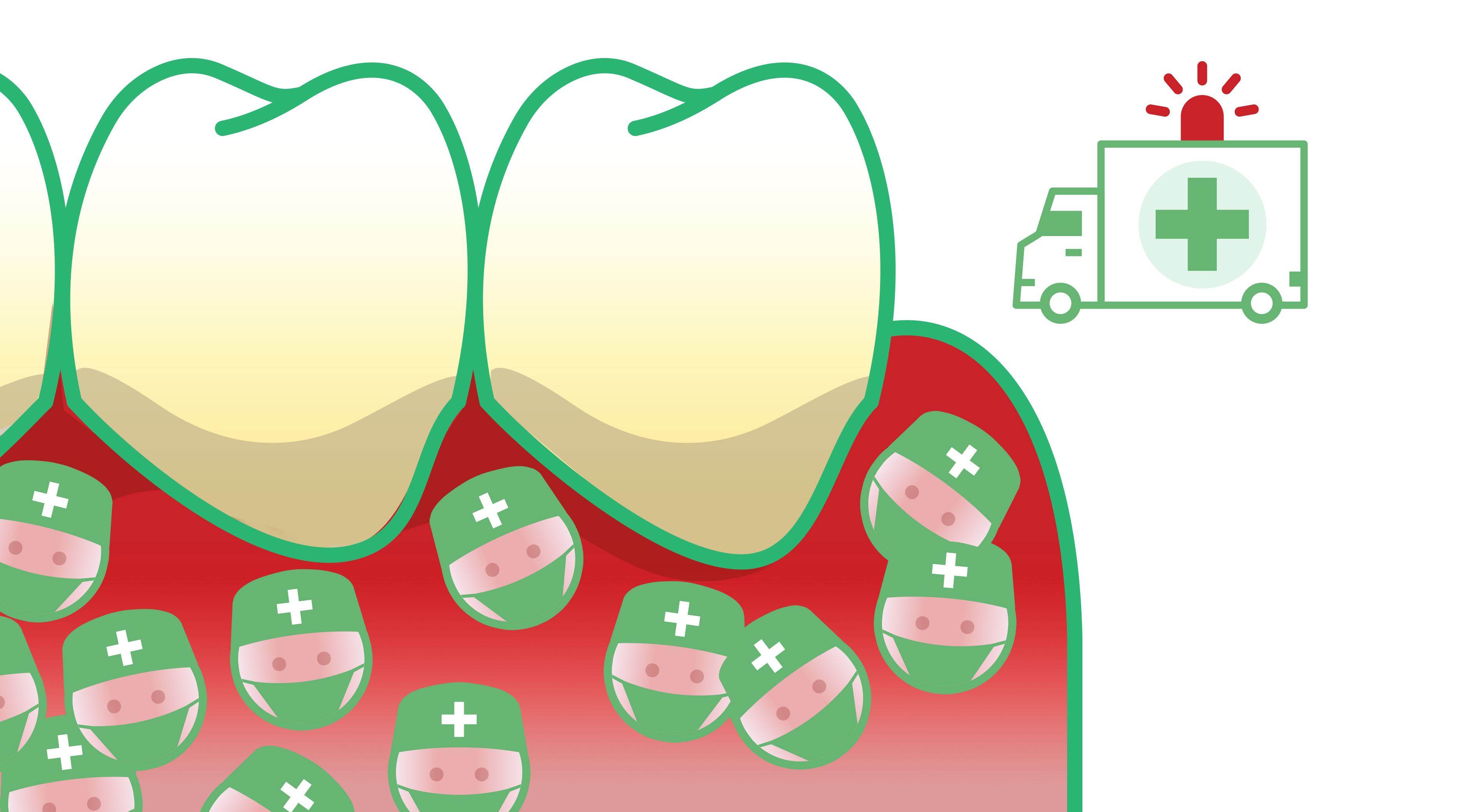
Over time, the persistent inflammation and the absence of reconstruction cause gums to pull away from the tooth and form pockets. Unlike healthy gums which act as a physical barrier, inflamed gums allow the attack from bacteria to heighten. Indeed, it becomes easier for bacteria to enter the tissue and “feed” the inflammation. With the immune cells involved in an ongoing battle against bacteria, the inflammation becomes self-perpetuating and the body goes into “inflammation overdrive”. Eventually, the immune cells’ efforts to kill the bacteria will also cause damage to the tissue [8]. You could call this collateral damage. With periodontitis, the bone and tissues supporting the teeth end up being destroyed [9]. This damage is irreversible and requires professional intervention to prevent eventual tooth loss [10].
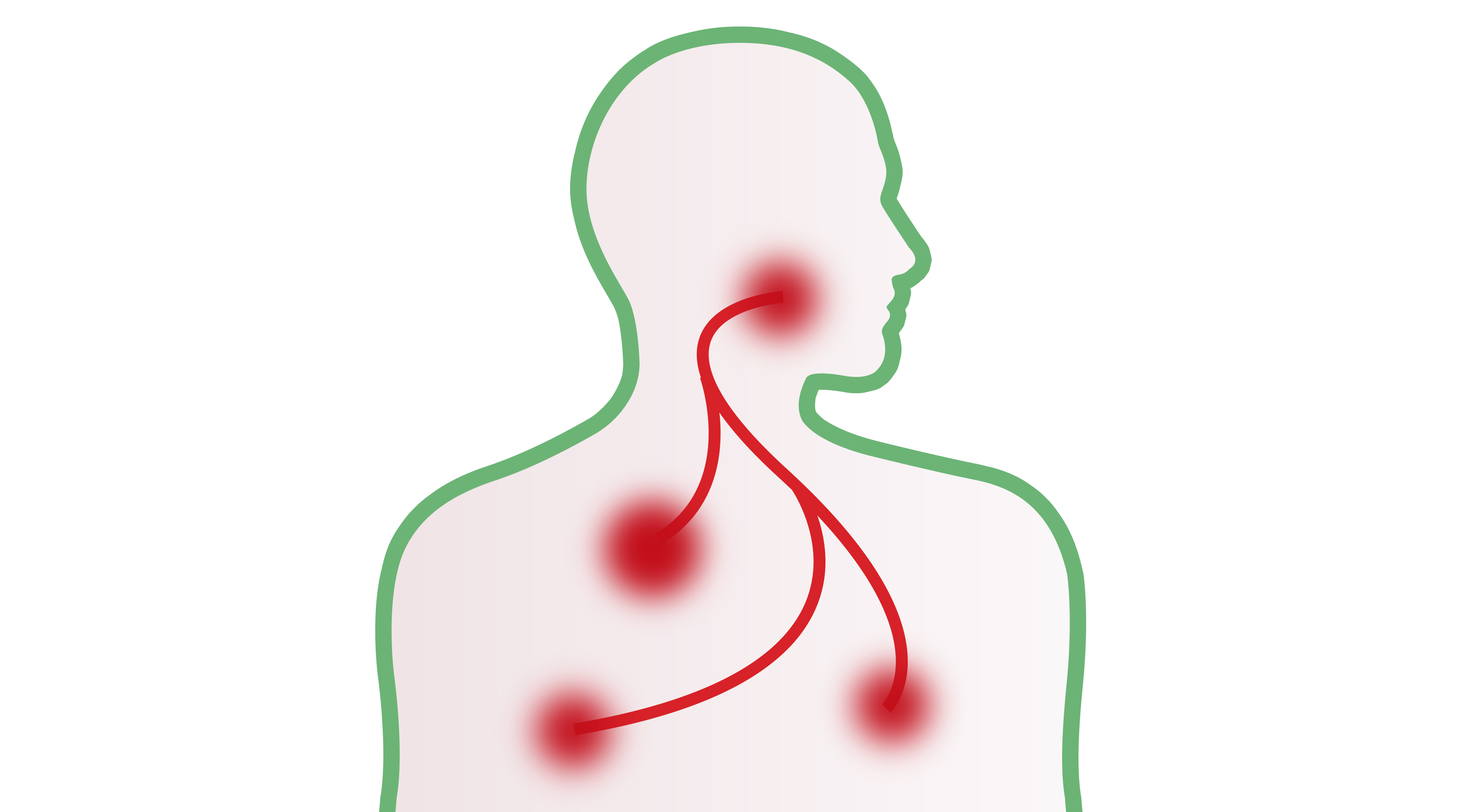
Chronic inflammation – the common denominator between periodontitis and systemic diseases
As we saw previously, periodontitis comes with severe consequences for your oral health. But, there is more to it. Chronic gum disease also puts your general health at stake. Indeed, inflammatory processes in one organ can cause or aggravate harmful processes in other organs or tissues [11]. There is a proven relationship between oral and general health problems, as stated by the World Oral Health Report (2003) [12]. Studies have produced interesting evidence relating to the link between periodontitis and heart attacks, diabetes and stroke [13].
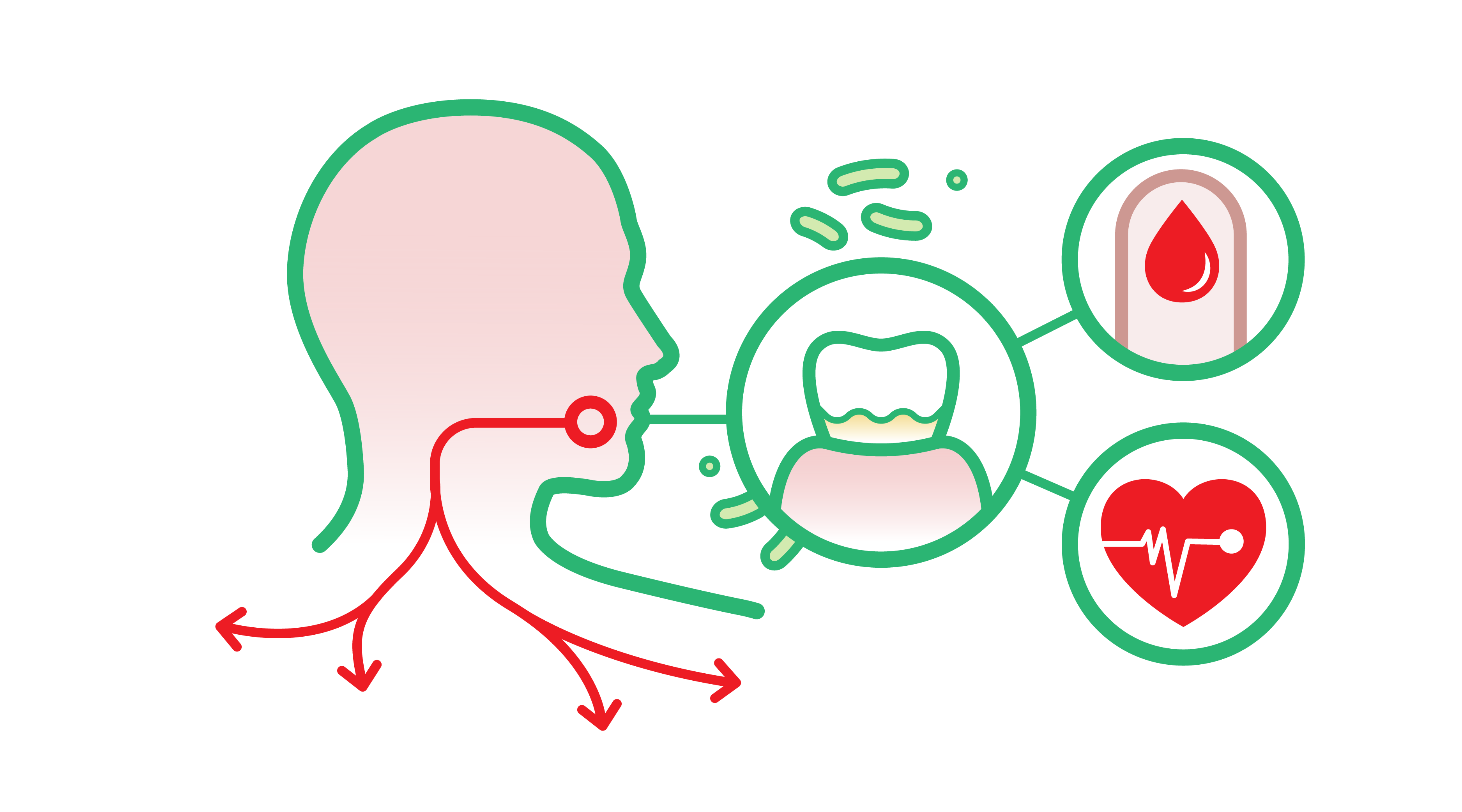
A study in Sweden found that hypertension and the prevalence of heart attacks were related to the severity of periodontitis, independent of age [14]. Periodontal disease has also been associated with stroke [15]. Regarding diabetes, there is evidence to show that the link is in fact bidirectional [16]. Indeed, studies have confirmed that periodontitis adversely affects blood sugar control in diabetic patients and increases the risk of complications, while diabetes increases both the prevalence and severity of periodontitis, particularly in cases of poor blood sugar control [17].
This relationship is explained by the fact that periodontitis and a number of systemic diseases share a common inflammation pathway. Inflammation is used to resolve localized damage but in fact consists of a whole-body reaction. Indeed, as the immune cells – called for reinforcement – travel through the body to reach the affected area, they can activate inflammation in other areas. In other words, inflammatory mediators released by these cells are able to “carry” the inflammatory response to other parts of the body, where they can cause or aggravate existing inflammation [18]. Chronic inflammation should be considered as a particular body state which promotes injuries and diseases. We told you that inflammation was a complex affair!
What should I take away from all this?
Protect your health - and oral health - by tackling gum inflammation before it becomes chronic
Chronic inflammation, tooth loss, systemic diseases…we touched on some serious topics. But remember, you don’t just wake up one day with chronic gum disease. It usually starts off as mild inflammation of the gums. If gingivitis isn’t treated and its root cause addressed, it will linger, worsen and eventually progress to periodontitis.
But that shouldn’t happen to you if you take good care of your oral health! Remember what we said: build-up of plaque around the gum line is one of the most important causes of gum inflammation [19]. Plaque is a soft biofilm [20]. It’s these bacteria that cause inflammation in the gums of susceptible individuals – the toxins they release come into contact with gum tissue, triggering an inflammatory-immune response. For more information on plaque, read our blog article. Plaque formation is an ongoing process so there’s no running away from it. The good news is you can easily take action.
What can I do?
Take up a complete oral care routine to keep plaque in check
If you have first signs of gum inflammation or are looking to prevent this, plaque removal needs to be your top priority. The most important thing is to take up a complete oral care routine. In case you didn’t know, this includes brushing, interdental cleaning and rinsing, to remove any leftover food particles.

First, interdental cleaning! This is crucial. Plaque tends to accumulate between the teeth, so if you’re determined to keep your gums healthy, you’ll want to be really disciplined with this.
The good news is there are plenty of great tools to help you with this: interdental brushes, rubber interdental picks or floss. Rubber picks are really gentle on your teeth and gums,and super easy to use. Whichever tool you use, what matters most is that you do it every single day, before brushing ideally.
Next up - brushing! You’re probably a good brusher already, but here are a few friendly reminders. Make sure you brush twice a day, for at least two minutes, using the appropriate technique. Always be gentle and use a soft toothbrush to avoid hurting your gums. If your gums feel a little tender, inflamed, or bleed when brushing, we suggest using a toothpaste from our GUM® PAROEX® range. If bleeding persists, you should consult your dentist.

The final step of your oral care routine should be rinsing. We recommend using a non-aggressive mouthwash which will help fight plaque without irritating your gums. If you’re dealing with gum inflammation, try a mouthwash from our GUM PAROEX range. Don’t forget to pay a visit to your oral care practitioner twice a year for a professional cleaning and personalized care.



Be mindful of your sugar intake
Any food you eat is going to contribute to plaque formation but sugary food and drinks are by far the worst. Our advice would be to limit your sugar intake if possible [21]. If you have a sweet tooth, we would suggest brushing your teeth after eating or drinking anything sugary. Raw, crunchy fruit and vegetables can also help dislodge plaque and food debris from between your teeth [22] so bear that in mind next time you have the choice between a celery stick and a chocolate bar! Chewing-gum can also do the trick.
Good to know
Plaque is the number one cause of inflammation but that doesn’t mean other factors don’t come into play. Smoking, stress, pregnancy and use of certain medication can increase your risks of developing gum inflammation [23]. While these factors aren’t all within your control, it’s good to be aware of them and to raise any concerns you might have with your oral care practitioner.
Protect your oral and overall health by stopping inflammation in its tracks
- Acute inflammation is the body’s response to harmful stimuli – it enables the healing process of damaged tissues and then disappears. Chronic inflammation, on the other hand, is persistent and self-perpetuating – it inhibits the healing process and causes further damage in the body. Make sure you address the root cause of acute inflammation to prevent it from lingering and getting worse.
- Chronic inflammation can spread… Starting off in one part of the body, it can then cause or aggravate inflammation in another part of the body. There is a proven relationship between periodontitis and systemic conditions such as heart attacks, stroke and diabetes. The better you protect your oral health, the better you protect your overall health.
- Gum inflammation often declares itself due to a build-up of plaque around the gum line. You can help prevent this by taking up a 3-step oral care routine and visiting your oral care practitioner twice a year.






